Penny Mordaunt has welcomed the Government’s announcement of a new research project that will expand the hugely successful HIV opt-out testing programme into areas with a high prevalence of HIV, including here in Portsmouth, to support its ambition to end new transmissions of HIV within England by 2030.
Penny commented: “This is a sensible decision by the Government to extended HIV opt-out testing to areas such as Portsmouth, with high HIV rates. We know that in trials this sort of testing not only saves lives, but also reduces pressure on our NHS, as early detection and intervention saves lives and money.
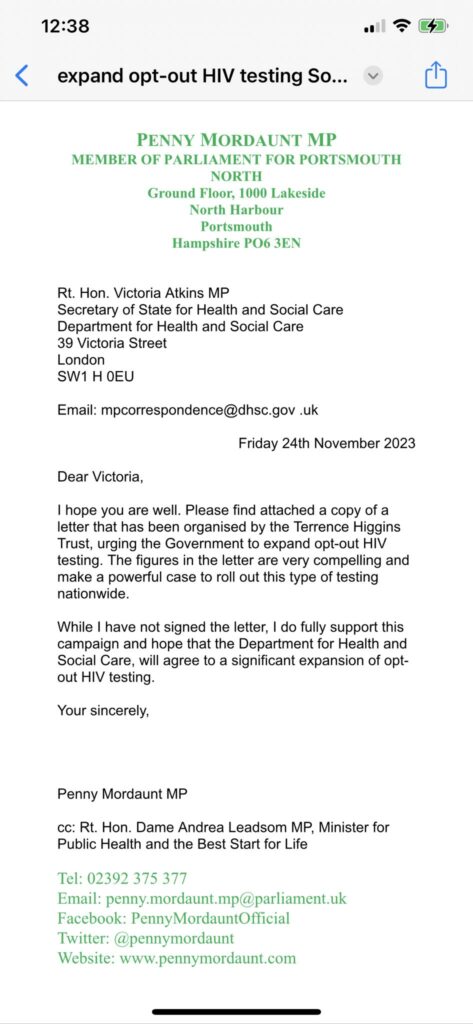
“The expansion of testing has been called for by medics, charities including the Terrence Higgins Trust and championed by a number of my colleagues locally.
“This is really good and as we mark world AIDS Day, shows the Government’s commitment to tackling deadly diseases like HIV.”
Backed by £20 million of funding from the National Institute for Health and Care Research (NIHR), the new project will expand efforts to detect undiagnosed HIV, Hepatitis B and C to 46 more emergency departments in England – into areas with a high prevalence of HIV.
The expanded programme could identify a significant proportion of the estimated 4,500 people living with undiagnosed HIV, preventing new transmissions and saving more lives.
Health and Social Care Secretary, Victoria Atkins commented: “Less than three decades ago, HIV could be a death sentence. It was often – and wrongly – considered a source of shame, and diagnoses were hidden from friends, family and society. But today, thanks to effective treatments, it is possible to live a long and healthy life with HIV.
“As well as promoting prevention for all, the more people we can diagnose, the more chance we have of ending new transmissions of the virus and the stigma wrongly attached to it.
“This programme, which improves people’s health and wellbeing, saves lives and money.”
Last year, as part of the Government’s world leading HIV Action Plan, NHS England launched the blood borne viruses (BBV) opt-out testing programme, with funding available for 34 emergency departments in areas with the highest prevalence of HIV. The announcement will mean the programme will be expanded as part of a research evaluation to 46 more emergency departments, covering 32 areas with a high prevalence of HIV.
The expansion will support the UK’s progress in being a world leader in the fight against HIV – and in meeting its goal to end all transmissions of HIV in England by 2030.
The evaluation of the expansion of opt-out testing will help reach the ambition set in January 2019 in reducing new HIV transmissions by 80% in 2025 and ending new transmissions by 2030, according to an update on the HIV Action Plan for England.
Professor Kevin Fenton, government’s Chief Advisor on HIV and Chair of HIV Action Plan Implementation Steering Group said:
“We know HIV is most commonly unknowingly spread by people who don’t know their status. Knowledge is power in preventing HIV transmission and accessing life-saving care.
“The core ambitions of our world-renowned HIV Action Plan are to intensify HIV prevention; expand HIV testing; strengthen linkage to and retention in high quality HIV care; and tackle HIV stigma and discrimination. We will not give up this fight until there are no new HIV transmissions in England.
“The opt-out testing programme will boost our progress to identify the estimated 4500 people who could be living with undiagnosed HIV and help us ensure we meet our 2030 ambition, with the possibility to save thousands of lives in the process.”
The existing programme, in extremely high prevalence areas, has been shown to be highly effective in identifying HIV in people unaware they had the virus and those who have become disengaged with care. The programme provides medication, a treatment and a care pathway, which enables people to live long and healthy lives – where the virus is virtually undetectable.
During the first 18 months of the BBV opt-out testing programme, 33 emergency departments conducted 857,117 HIV tests, 473,723 HCV tests, and 366,722 HBV tests – significantly increasing the number of blood borne virus tests conducted in England each year. These tests have identified:
· 569 people living with HIV and 345 people disengaged from HIV care.
· 2,206 people living with HBV and 388 disengaged from HBV care.
· 867 people living with HCV and 186 disengaged from HCV care.
Anne Aslett, CEO of the Elton John AIDS Foundation: “The Elton John AIDS Foundation launched the first HIV Social Impact Bond in 2018 because too many vulnerable people were being left behind. Together with our partners, we identified opt-out testing in emergency departments as an effective, and cost-saving, way of ensuring people living with HIV get the treatment they needed.
“We warmly welcomed the Government’s decision to expand this successful method of HIV diagnosis to 33 sites in April last year and results from the last 18 months demonstrate how incredibly important this approach is to ensure no one is left behind. This week’s announcement to further expand opt-out testing to 46 additional emergency departments is another fantastic and very significant step towards meeting the goal of ending new HIV transmissions by 2030 and above all else will save lives.”
Outside of BBV opt-out testing, progress is being made. There are fewer people living with undiagnosed HIV, while new HIV diagnoses remain much lower than their peak. As a result of effective treatments, it is possible to live a long and healthy life with HIV. Most people with HIV diagnoses are receiving world class treatment, making it undetectable.
There is much to celebrate, ahead of World AIDS Day (1 December), with progress made towards the Action Plan, with fewer than 4,500 people living with undiagnosed HIV – the lowest it’s ever been since recording begun – and extremely high levels of antiretroviral treatment, used to treat HIV, and viral suppression.
In 2022, England once again achieved the UN AIDS 95-95-95 target nationally. 95% of people living with HIV being diagnosed, 98% of those diagnosed being on treatment and 98% of those on treatment having an undetectable viral load – meaning the levels of HIV are so low, that the virus cannot be passed on.
In a speech at the All Party Parliamentary Group on HIV and AIDS event to mark the launch of the new project, Health and Social Care Secretary Victoria Atkins thanked the ongoing dedication from NHS staff, HIV charities and campaigners, which have worked tirelessly to support the government in achieving its goal to end new transmissions.
People with reactive/positive tests results are linked to care and offered information and support through community organisations.
The opt-out strategy for BBV testing is important to address health inequalities by reaching groups, such as those from ethnic minorities or women, who are less likely to attend sexual health services and may be disproportionately affected both by higher rates of some BBVs and stigma associated with BBV testing or diagnosis.
Opt-out testing additionally provides a valuable opportunity to re-engage with people who have previously been diagnosed with a BBV but who are not accessing treatment or care.
Richard Angell, Chief Executive of Terrence Higgins Trust, added: “Yesterday’s announcement is the turbo boost we need if we are to end new HIV cases by 2030. It’s hugely welcome that an additional four million HIV tests will be carried out in A&Es over the next year thanks to a temporary but wholesale expansion of opt-out HIV testing. This landmark investment to triple HIV testing in England – from 2.5 million tests a year to 6.5 million – is absolutely crucial to find the 4,400 people still undiagnosed.
“The evidence is crystal clear: testing everyone having a blood test in Emergency Departments for HIV works. It helps diagnose people who wouldn’t have been reached via any other testing route and who have often been missed before. It also saves the NHS millions, relieves pressure on the health service and helps to address inequalities with those diagnosed in A&E more likely to be of Black ethnicity, women and older people.”